TL;DR;
You don’t need to dive into the AI wave head first in order to reap the benefits of commoditized AI.
- AI analytics use cases around classification (e.g. social needs identification, patient sentiment analysis, program eligibility) offer low lift, moderate impact opportunities.
- Mature, widely available tools & methods can simplify adoption and integration into existing analytical workflows.
- Established and well-documented model evaluation methods reduce complexity while building stakeholder trust in AI capabilities.
Advances in AI continue to outpace practical adoption, but health centers and primary care organizations don’t need cutting-edge tech to benefit and make meaningful improvements in population health with analytics powered by commoditized AI. We’ve had these analytics use cases in mind since the GPT 3.5 days, and I believe they are still extremely relevant as low lift, moderate impact applications of AI that can make a real difference.
Social Drivers Identification
Social drivers account for up to 80-90% of modifiable contributors to health outcomes. While structured data collection of social drivers (e.g., Z-codes) is increasing, many social needs remain hidden in free-text EHR notes. In 2024, 60% of family physicians still used free-text notes to document social needs in their EHR. That’s almost 2x higher than the use of diagnosis codes alone.
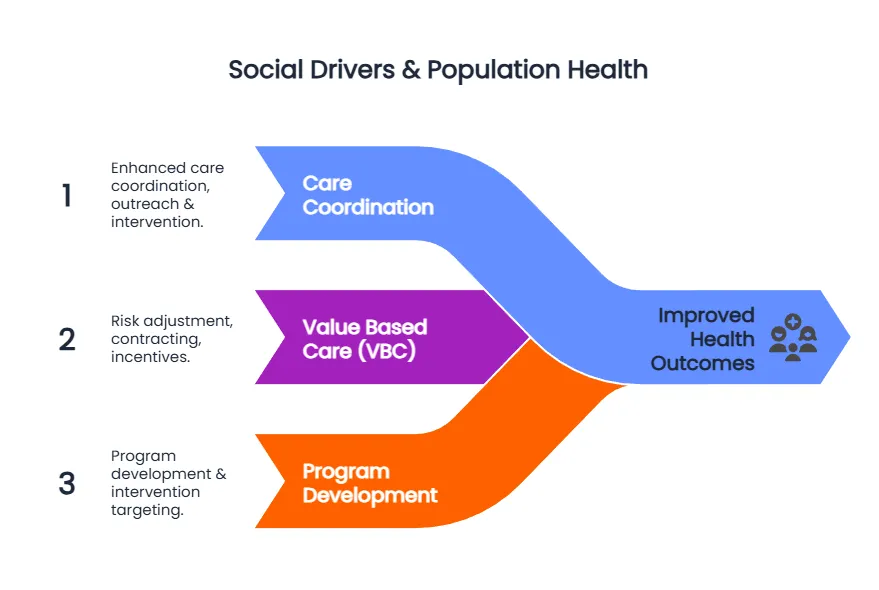
AI-driven extraction of social needs can support population health management at scale. It traverses strategy and execution through:
- Enhanced care coordination & resource allocation: identifying social risks, such as housing or food instability, can help the care team connect patients with community supports, while focusing outreach & engagement on areas of greatest need.
- Equitable value-based care: social drivers can impact risk adjustment, segmentation & risk stratification, inform contracting, and improve performance under value-based frameworks.
- Agile Programs & Interventions: enhanced community & individual-level drivers can inform rapid program development and identify pivot points.
For states like California, where addressing social drivers is part of the Medicaid (Medi-Cal) system via CalAIM, identifying patients with undiagnosed (yet documented) health-related social needs can expand the landscape of services patients may be able to receive. CalAIM revolves around a series of populations of focus, many with likely complex social needs:
- Individuals and Families Experiencing Homelessness.
- Adult High Utilizers.
- Adult Serious Mental Illness (SMI)/SUD.
- Individuals Transitioning from Incarceration.
- Individuals at Risk for Institutionalization and Eligible for Long-Term Care Services.
- Nursing Facility Residents Who Want to Transition to the Community.
These populations can benefit from community supports such as: housing transition navigation services, housing deposits, housing tenancy and sustaining services, short-term post-hospitalization housing, medically-supportive food, sobering centers, asthma remediation and more.
Patient Experience Sentiment Analysis
Successful population health depends on strong, long-lasting patient relationships. Exceptional patient experiences lead to improved patient engagement, better treatment adherence, and enhanced continuity of care. From a value-based care standpoint, good patient experiences lead to improved patient retention, which in turn gives primary care systems the opportunity to reap the benefits of population health management programs that can take 2+ years to materialize (if you’re in the prevention game, it can take even longer).
Traditional surveys (i.e. CAHPS) provide valuable, standardized information for tracking, but lack the fidelity to be useful for service recovery and just-in-time pivots. If any patient interaction as one that will generate a patient experience, a treasure trove of data can then help us identify and resolve pain-points closer to real-time.
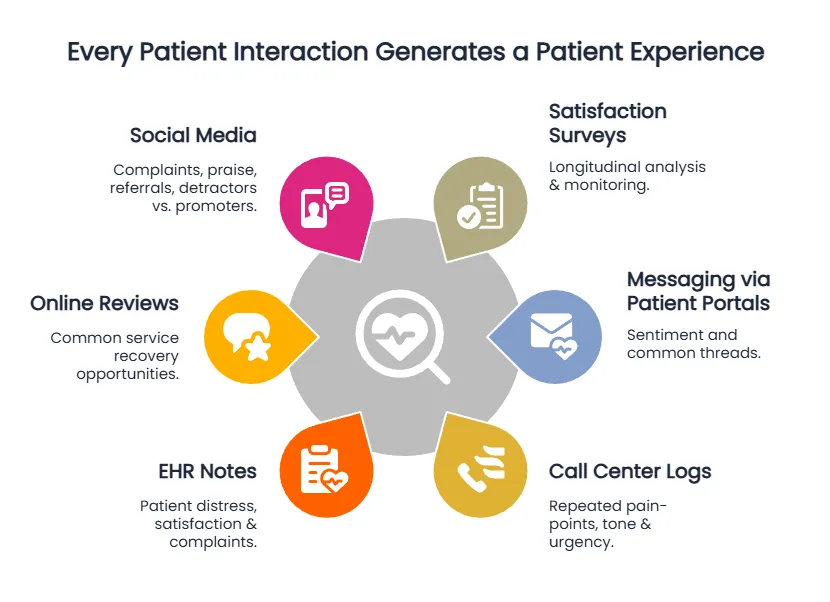
As the universe of methods to collect and understand patient experiences expands, so do the practical use cases that move beyond standardized surveys:
- Real-Time Service Recovery: AI-driven sentiment analysis of patient feedback can enable rapid identification of negative experiences, allowing for timely outreach & issue resolution.
- Operational Insight & Improvement: categorizing sentiment into operational themes (i.e. wait times, staff courtesy, scheduling, facilities) can provide actionable insights to prioritize operational adjustments and improve workflows.
- Provider Performance & Training: individual & aggregate patient-provider interactions can guide individualized coaching and training programs, helping providers and care teams refine the patient experience.
- Health Equity: segmenting sentiment data can highlight disparities or differences across patient populations.
AI Patient Identification for Programs/Services
Optimizing interventions for high-needs high cost (HNHC) patients starts with identifying and targeting the right patients. This can be resource-intensive and significantly expensive, leading to missed opportunities for patients that could see benefits from programs.
Commoditized AI tools can power automated chart summarization and rapid eligibility screening to uncover and prioritize eligible patient populations, reduce the administrative burden, and allow care teams to redirect their focus to patient engagement. In resource-constrained environments, a data & AI-driven proactive identification approach can help focus resources on the critical few.
Blending traditional & heuristic/deterministic data & analytics methods with AI classification can yield better insights to inform & drive:
- Medication-assisted treatment (MAT) for substance use disorders: AI classification can identify disorders informally documented in clinical notes or historical encounters, enabling proactive outreach.
- Home accessibility & community supports referrals: identify patients with documented but uncoded mobility, safety, accessibility, or health-related social needs to drive referrals to community supports & improve patient safety.
- Post-discharge follow-up & prioritization: discharge note summarization and classification can identify key factors indicative of high risk of readmission or complications, enabling care teams to prioritize follow-up outreach for higher-risk patients.
- New member segmentation ahead of a first visit: summarize historical encounters & the longitudinal medical record to stratify, segment, and prioritize new members ahead of a first encounter.
Great, But How?
Analytically, these use cases represent low lift opportunities due to a few factors:
- Cross-use-case transferability: these use cases are different flavors of the same core concept - text classification.
- Low barriers to entry: the tools to leverage AI in this context are mature and many are already embedded in existing applications (python, R, Big Query, Databricks, etc.).
- Reusable evaluation methods: methods to evaluate performance & accuracy are well known and can be reused from traditional ML use cases.
Text Classification: Same Concepts, Different Flavors
Whether performing sentiment analysis on online reviews, summarizing a patient’s medical record, or identifying a patient’s unhoused status, they all depend on the same core concepts:
- Analytics methods & paradigms for processing unstructured data - embeddings, tokenization, named-entity recognition, etc.).
- Prompt engineering & orchestration for extracting structured insights from free-text.
- Iteration through training, testing, evaluation, production deployment.
Mature Tools: Same Development Environment
A majority of AI models (whether paid or open source, cloud-based or local) can already be leveraged in existing platforms and tools, with lower training overhead.
- Python: there is no shortage of AI frameworks for Python - from more established products like LangChain, to newer entrants to the market, like Letta & Agno.
- R: although still catching up, R already has a variety of packages for interacting with LLMs, from the tidyverse variety in ellmer, to more dplyr-like options like tidyllm or mall.
- For cloud-based platforms, products like BigQuery & Databricks have implemented AI functions right into SQL, bringing the power of LLMs right into your SQL queries.
What this ultimately means is less time spent on new software, and more time spent on rapid prototyping, proof-of-concept development, and production deployment.
AI Evaluation: Reusing What We Already Know
Your typical evaluation metrics for text classification (accuracy, precision, recall, F1-score) remain consistent across these use cases, making evaluation accessible and well-documented.
While traditional methods remain relevant, the mechanics of evaluation can leverage AI itself to evaluate performance. This opens up a variety of new options, including:
- LLM as judge - LLMs used to score output and track model performance over time (indeed, quite the tropical option).
- Pairwise evaluators - leverage multiple models for classification and battle it out in a chatbot arena.
Conclusion
Harnessing commoditized AI for population health doesn’t require full-scale technological overhauls, or deep pockets. By pragmatically leveraging accessible AI methods in text classification and NLP, health systems can achieve meaningful impacts on patient care, operational efficiency, and health equity today, without going head first into the AI wave. These AI-driven use cases represent realistic opportunities to rapidly enhance how organizations leverage analytics to execute on strategy, and drive benefits for communities and care teams alike.